Understanding Diabetes
Type 1 diabetes (T1D) develops when the immune system attacks the cells in the pancreas that make insulin. T1D most commonly develops in children or young adults, and there is no way to prevent or cure T1D. Type 2 diabetes (T2D) occurs when the pancreas cannot create insulin in the proper amount for blood sugar management or when the body may not use the insulin it has correctly. As a result, blood sugar levels increase to unsafe levels.

More than 37 million Americans have diabetes.
5-10% of diagnosed cases have Type 1 diabetes.
90-95% of diagnosed cases have Type 2 diabetes.
When diabetes is not controlled, patients’ high glucose levels can lead to serious health complications and even death. In fact, diabetes is the 7th-leading cause of death in the United States. There are 96 million U.S. adults – more than 1/3 of the population – who are living with prediabetes, and more than 80% of these adults do not know they have it.
How Diabetes Impacts Health
Over time, diabetes can damage the heart, blood vessels, eyes, kidneys, and nerves.

Adults with diabetes have an increased risk (2x-4x) of strokes and heart disease.

Combined with reduced blood flow, nerve damage in the feet increases the chance of foot ulcers, infection, and amputation. In fact, more than 60% of non-traumatic lower-limb amputations are in patients with diabetes.

Diabetic retinopathy is a cause of blindness as a result of long-term accumulated damage to the small blood vessels in the retina.

Diabetes is among the leading causes of kidney failure.

People with diabetes are more likely to have poor outcomes for several infectious diseases, including COVID-19.
Medtech’s Role in Improving Diabetes Care
Early diagnosis and treatment of diabetes can lead to improvements in long-term health outcomes of patients. AdvaMed® members are developing new devices and technologies that make day-to-day life healthier and easier for those living with diabetes – and allow patients to manage their diabetes more effectively, improving their care outcomes in the process. These include continuous glucose monitors (CGMs), which automatically track glucose levels day and night, allowing persons with diabetes to see where their glucose values have been, where they are now, and where they are going, with fewer or no finger sticks compared to the older traditional blood glucose monitors.
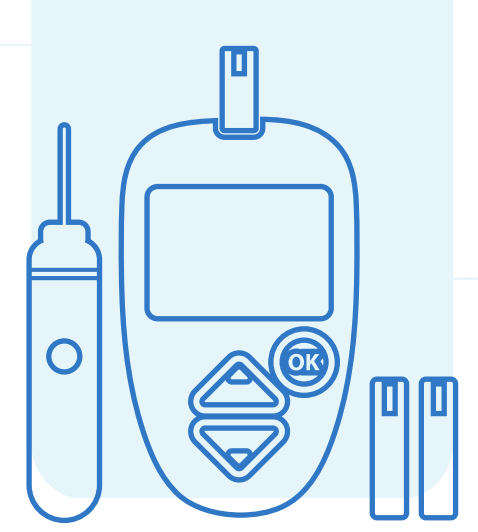
The most common alternative to CGMs, a method called blood glucose monitoring (BGM), only provides point-in-time data and often misses important high or low blood glucose level episodes. Thanks to advancements in medical technology, CGMs can fill in important data gaps and even alert the patient in real time of a high or low glucose episode so they can immediately bring their glucose back into an optimal range. CGMs generally consist of a sensor/transmitter that is worn on the body to measure glucose data and a reader or smartphone that allows users to view current and past glucose readings.

CGMs are often used with insulin pumps, which are small, computerized devices that deliver insulin in small doses or a bolus dose close to mealtime to control the rise of blood sugar after a meal, mimicking the body’s normal release of insulin.
The next generation of these advanced diabetes technologies will link CGM and insulin pump use together through an algorithm to create an artificial pancreas, so that patients will be able to count on their CGM to let the insulin pump know when insulin is needed. It will be crucial in the near future for private health plans and public programs like Medicare to bring clarity to their coverage and payment policies for technologies like the artificial pancreas.


